Did you know that the ‘gut feeling’ or the ‘butterflies’ that you feel in your tummy are more than just random physical symptoms? They are more of a description of your body’s reaction to your surroundings and your brain decoding nonverbal or emotional cues. Often called the ‘second brain’, the gut is an intricate network of neurons that works tirelessly to digest food, absorb nutrients and push out products that your body doesn't need.
Your gut is also home to several bacterial species called ‘microbiomes’ that make up the gastrointestinal tract. These microbiomes are a good kind of bacteria that regulate digestion and metabolism. Not to forget, they build the gut wall to keep out unwanted microbes and release antimicrobial chemicals that shield the body against pathogens.
At the same time, the microbiomes living in your gut affect more than just your physical health. Over the years, there's been mounting scientific evidence that highlights their ability to communicate with the brain – often referred to as the gut-brain connection – and thereby your mood.
In the wake of the close interactions between the gut and the brain, it is now easier to understand why one feels nauseous right before giving a speech in public or an intestinal pain during stressful times.
How does your gut talk to the brain?
The human body is an amazing machine that has simultaneous communication channels running between different parts of the body 24×7. When talking about your gut and brain, there are two key-ways in which they interact:
1. Via the vagus nerve
The longest of the 12 cranial nerves, the vagus nerve monitors the functioning of internal organs. So, there's little that doesn't come under its KRA. The brain and the large intestine are two of the several body parts that the vagus nerve connects. Scientific research has revealed that what happens in the gut can control your brain and mood via the vagus nerve.
“The brain-gut axis is becoming increasingly important as a therapeutic target for psychiatric gastrointestinal disorders, such as depression, inflammatory bowel disease (IBD), and post-traumatic stress disorder (PTSD). The gut is an important control center of the immune system, and the vagus nerve controls that and has immunomodulatory properties. As a result, this nerve plays an important role in the relationship between the gut, the brain, and inflammation. For instance, vagal nerve stimulation is emerging as a potential non-pharmacologic strategy for the treatment of irritable bowel syndrome and abdominal pain. Singing, humming, gargling, and chanting activate the muscles at the back of vocal cords and throat connected to the vagus nerve, thereby improving symptoms,” says Dr Sandeep Thakur, Internal Medicine, HCL Healthcare.
The Immune system
One of the most persuasive links between mental health and the gut is related to our immune system. Apart from shielding the body against germs, the immune system also transmits complex brain signals to other body parts. As around 70% of the immune system is located in the gut, it responds to these signals – including those sent by the microbiomes – in real-time. The bidirectional communication between microbiomes and the immune system influences both of them. So, when you feel ‘gut-wrenched’, it’s a troubled brain’s signal to your gut. Likewise, stomach issues can be both the cause or a product of depression, stress, or anxiety. That's because of intertwining your gut and mood.
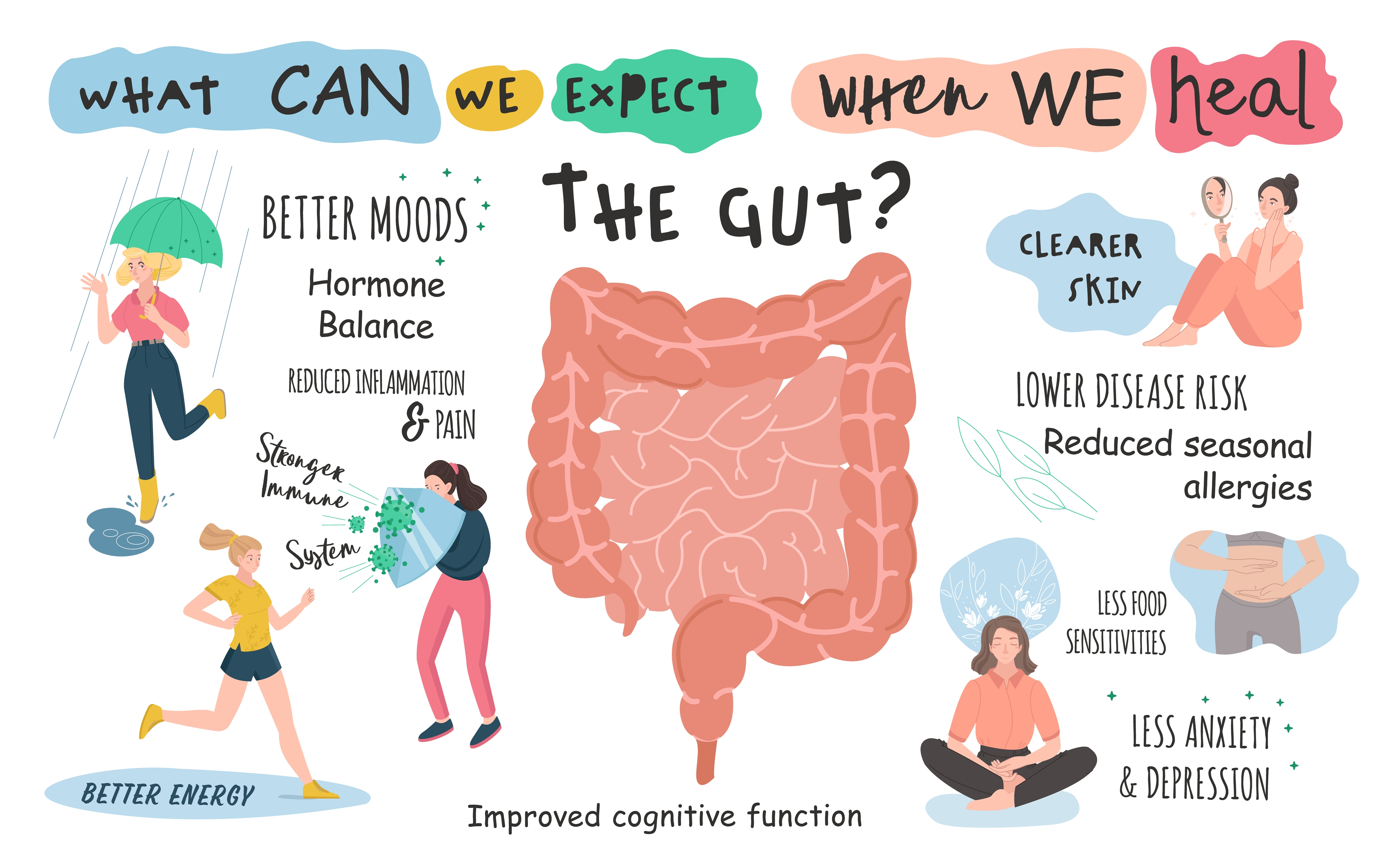
But how does your gut health dictate your mood? It's important to mention that around 90% of serotonin receptors are located in the intestine. Serotonin is a neurotransmitter that relays signals between nerve cells and affects emotions and mood. Medical fields like nutritional psychiatry are unraveling how your gut health can impact your mood. In fact, when a person is prescribed antidepressants, the most common side effects are related to the gut including diarrhea and gastrointestinal issues.
What you eat is how you feel.
The gut-brain axis offers a deep understanding of how any disruption in the activity of microbiomes affects one's gut health and mood. To avoid such disruptions, medical experts recommend a well-balanced diet that minimizes the consumption of processed and ultra-processed food, which are known to trigger inflammation and diseases.
“Hippocrates said all diseases begin in the gut. Your diet plays a crucial role in maintaining the health of the gut. Early colonization of good bacteria can help the gut ecosystem to function properly as these good bacteria help our bodies digest food and absorb nutrients, and even they produce several vitamins in the intestinal tract,” says Kirti Tandon, Quality Analyst (Dietetics), HCL Healthcare.
Here are some other ways in which you can get a healthier gut:
- Cut down on packaged and processed foods. The additives and preservatives in packaged foods tend to disrupt the healthy bacteria in your gut.
- Rather than opting for juices, try going for fresh vegetables and fruits. You can also try frozen fruits, provided they don't have added sugars or additives.
- Up the fiber content of your food. This can be easily done by increasing the number of whole foods or legumes in your diet.
- Try including probiotic-rich foods such as curd or even plain yogurt to your means. Probiotics are live microorganisms that provide health benefits when consumed, generally by improving or restoring the gut flora. It supports digestion as it supports a healthy gut microbiome, and further prevents gut inflammation and other intestinal problems.
- If you are non-vegetarian, eating less red meat and opting for a balanced meal to include lean poultry and seafood can go a long way in improving your gut health.
While these suggestions can help you boost the healthy bacteria in your gut, they are not a sustainable solution for chronic mental health problems like depression or anxiety. There's no dietary suggestion that can replace a doctor which is why it is important to seek medical attention at the right time.